Wait … the wrong incontinence care can lead to nursing care?
The Unicharm Incontinence Care Lab is working hard to create a world where seniors can live long, healthy, independent lives. As part of our efforts, we’re actively forging partnerships with local governments and various private groups to offer urinary incontinence seminars, presentations, and other learning opportunities to seniors in the general community.
The groups that sponsor these incontinence seminars are eager to host them, explaining that seniors are extremely interested in how they can help prevent the need for nursing care or avoid becoming homebound. This shows that people are aware that incontinence care is one of the keys to healthy senior living.
What about you? Are you concerned that you might end up needing nursing care if you do not address your incontinence issues? What is the relationship between urinary incontinence and nursing care? Read on to find out.
Does urinary incontinence make nursing care necessary?
The purpose of nursing care is to support the activities of daily living for seniors with physical limitations—meaning that they cannot live as they please. If a person with full physical functioning experiences urinary incontinence, it may be inconvenient (more trips to the bathroom and dealing with pad changes), but it shouldn’t seriously restrict daily life.
In other words, urinary incontinence by itself does not signal the beginning of nursing care.
Can urinary incontinence lead to nursing care?
That said, urinary incontinence can lead to nursing care if a person starts changing their life as a result.
If the incontinence worsens, it means even more trips to the bathroom, constantly looking for restrooms outside the home, needing to frequently use the restroom at other people’s homes, and so on—all of which causes psychological stress that can make people avoid going out entirely. This means fewer opportunities to meet people and more time spent at home, which in turn means less physical movement and decreased muscle mass. If the trend continues, the person could even end up needing nursing care.
Being homebound can also lead to dementia.
The problem is not addressing incontinence properly.
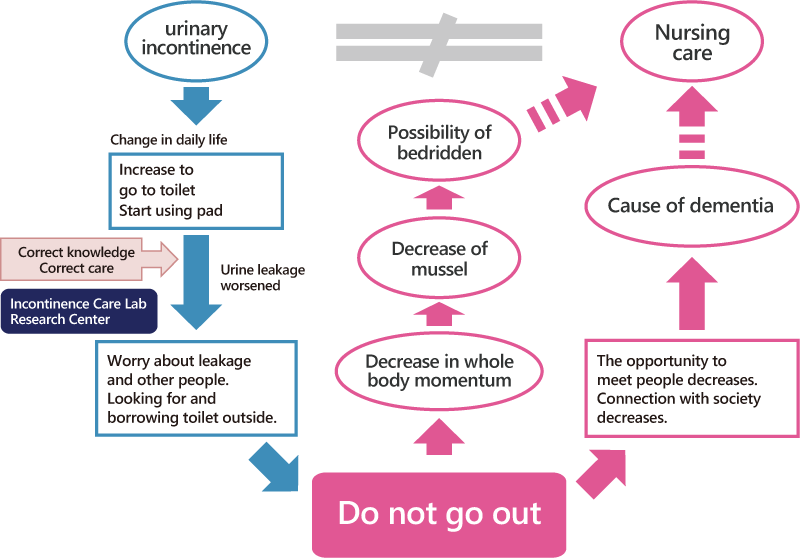
The problem is not the urinary incontinence itself, rather it is not tackling the problem in the right way.
People who take proper steps to address their urinary incontinence—wearing pads when they’re out and are concerned about finding a toilet, choosing highly absorbent pads when they’re concerned about major leaks, doing exercises to reduce leaks, or even seeking treatment from a physician—are able to stop the trend that can lead to the need for nursing care.
The purpose of incontinence care seminars is to help people realize that taking the right approach to leaks at the right time means that seniors can still continue living their lives with confidence.
The participants in these seminars have given us a lot of feedback about the importance of proper incontinence care. Read on to hear what some of them had to say.
Participant feedback from incontinence care seminars
“It’s not something I feel comfortable talking about myself, so it was great to learn about it in this format.”
“I was using menstrual pads to manage my leaks and had no idea that the products designed for incontinence worked so well. I’ll definitely use incontinence products from now on.”
“I’m going to be doing pelvic floor exercises every day now to help prevent leaks.”
“Now that I know what’s going on in the body that causes leaks, I understand better the importance of addressing them.”
“I had no idea they made these handy pads. Now I’ll able to go out and travel again.”
“I had no idea you could go to a clinic for urinary incontinence.”
Everyone had their own discoveries and realizations during the seminar, but all of them came away with less anxiety and a better understanding of proper incontinence care.
According to Dr. Kumiko Kato at the Japan Red Cross Nagoya Daiichi Hospital, who has overseen the development of the urinary incontinence care navigator, people vary widely in how long they wait to consult the urology department at Nagoya Daiichi after experiencing incontinence symptoms: from 6 months to 34 years, with an average of 9.1 years (±8). There were 113 patients (64%) who waited 5 years or more, while another 76 (43%) waited 10 years or more. Clearly people are silently struggling with incontinence on their own for a very long time without consulting a professional. By promoting proper awareness and care, we hope to end that silent struggle sooner.